Alzheimer’s Disease | Having a Sleep Disorder may increase risk

 Sleep disordered breathing and obstructive sleep apnea (OSA) are associated with biomarkers for Alzheimer’s disease, according to research presented at the Alzheimer’s Association International Conference 2017 in London.
Sleep disordered breathing and obstructive sleep apnea (OSA) are associated with biomarkers for Alzheimer’s disease, according to research presented at the Alzheimer’s Association International Conference 2017 in London.
Investigators found that sleep-disordered breathing increased the accumulation rate of brain β-amyloid in cognitively normal persons and in individuals with mild cognitive impairment. Another study found that obstructive sleep apnea (OSA) was associated with increased brain β-amyloid deposition, decreased cerebrospinal fluid (CSF) levels of β-amyloid, and increased tau protein levels.
Researchers at Wheaton College in Illinois conducted 3 studies that examined sleep patterns among participants in the Alzheimer's Disease Neuroimaging Initiative (ADNI) to characterize the potential effects of sleep-disordered breathing and OSA on brain changes associated with mild cognitive impairment and Alzheimer's disease.
In one study, Amanda Shim and colleagues examined brain β-amyloid-42 (Aβ42) accumulation in 516 cognitively normal subjects and found that those with sleep-disordered breathing had higher levels of CSF at baseline and a more rapid accumulation over time. No interactive effect was observed between OSA and APOE-e4, a risk gene for Alzheimer’s disease, suggesting that OSA may be independently associated with brain amyloid burden.
Megan Hogan and colleagues assessed the effects of OSA in 798 subjects with mild cognitive impairment (MCI). Similar to the cognitively normal cohort, baseline β-amyloid-42 levels and the rate of accumulation were higher in patients with OSA. These results, according to the investigators, suggest that sleep-disordered breathing may be an independent risk factor for Alzheimer’s disease and that interventions aimed at treating sleep-disordered breathing may also lower the risk for Alzheimer's disease. A combined analysis of the cognitively normal and mild cognitive impairment groups, as well as a third group with Alzheimer's disease (n=325), assessed the effects of OSA on levels of several Alzheimer's disease biomarkers in CSF and brain β-amyloid burden as measured with positron emission tomography. The findings included:
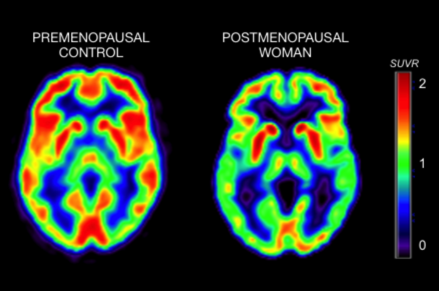
A combined analysis of the cognitively normal and mild cognitive impairment groups, as well as a third group with Alzheimer's disease (n=325), assessed the effects of OSA on levels of several Alzheimer's disease biomarkers in CSF and brain β-amyloid burden as measured with positron emission tomography. The findings included:
- Associations between OSA and CSF Aβ42 levels in the MCI and Alzheimer's groups.
- Significant OSA associations with brain Aβ42 levels in cognitively normal persons and those with MCI.
- OSA patients had a faster increase in brain Aβ42 over time in the cognitively normal and MCI groups.
- OSA patients had a faster decrease in CSF Aβ42 and increases in tau and p-tau volumes over time in both the cognitively normal and MCI groups.
The results “highlight the importance of checking for, and accurately diagnosing, sleep-disordered breathing, especially in people at risk for dementia, and more importantly in people diagnosed with MCI, so that it can be addressed and treated,” said research team leader Omonigho Bubu, MD, MPH.