APRN Minnesota | Nurse Practitioner definition and purpose
 Senate bill 511 in Minnesota | What is really being said here? Solving the shortage and continuing to deliver quality care, or is this really a power struggle?
Senate bill 511 in Minnesota | What is really being said here? Solving the shortage and continuing to deliver quality care, or is this really a power struggle?
What we have here is a power struggle. Nurse Practitioners have proved themselves since their inception (brought on by physicians themselves who needed additional expertise and support to deliver care).
Imagine that the title of ‘Nurse Practitioner’ were really something more associated with delivering quality care, improving access, and meeting the needs of today’s physician shortage. Because that is what it is. What is a practitioner?
- thesaurus.com expresses ‘practitioner’ as a noun, an expert.
- Additional terms: doctor, professional, pro, master, specialist.
- ‘Someone who practices a profession or an art’, from the World English Dictionary.
Call the profession for what it is, not what the perceived power struggle is, that just leads to confusion and name calling.
In the latest article from fiercehealthcare.com. putting the real question to both sides ‘Do differences in physician and NP training impact patient care?’
[As more states expand the scope of practice for nurse practitioners (NPs) in an effort to combat the growing physician shortage, Remapping Debate explores the differences in training between the providers and whether those differences impact patient care.
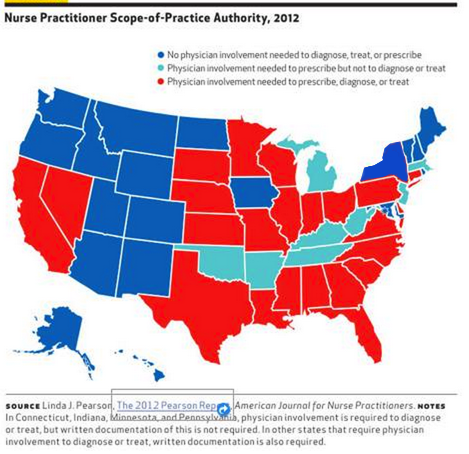
Sixteen states and the District of Columbia currently allow NPs to practice independently rather than under the supervision of a physician, according to the article. But many physicians object to the expanded scope of practice, claiming it jeopardizes team-based care and that NPs don't have the depth of education and training necessary for complex medical decision-making.
 Although a 2013 poll indicates that Americans believe that NPs should have greater freedom to provide healthcare services, physicians interviewed by Remapping Debate say that while NPs are able to treat common conditions, doctors are better able to manage patients with multiple, complex conditions and act as mediators between a patient and specialists.
Although a 2013 poll indicates that Americans believe that NPs should have greater freedom to provide healthcare services, physicians interviewed by Remapping Debate say that while NPs are able to treat common conditions, doctors are better able to manage patients with multiple, complex conditions and act as mediators between a patient and specialists.
The differences in care are due in part to the education and training physicians receive compared to NPs, according to the article. Doctors must complete a four-year graduate degree as well as a three-year residency program in a hospital or clinical setting and have approximately 15,000 hours of combined clinical training under their belt before obtaining their medical licenses. But in order to receive their licenses, NPs must obtain one or two graduate degrees, which typically require 500 to 700 hours of clinical practice.
NPs interviewed by Remapping Debate say that the extra hours of doctor training makes physicians "different primary care providers," and not necessarily "superior" ones. They also pointed to studies that conclude that patients treated by NPs have similar outcomes than those under the care of doctors and in some cases, NPs receive higher patient satisfaction ratings.
But physicians in the article say the studies often fail to distinguish between care provided by NPs independently and care provided under some sort of collaborative relationship with a doctor. Furthermore, they say the case studies only track patients for a few months or those with common conditions, and miss long-term complications or complexities in the diagnostic process.
![]() NPs, however, say there is no evidence to support that their diagnostic abilities aren't up to par or they have higher rates of midiagnosis. "If we could not recognize [such cases], you would see a lot more lawsuits against nurse practitioners for not recognizing them, but those lawsuits aren't there," Angela Golden, a clinical nurse practitioner and educator and co-president of the American Association of Nurse Practitioners told Remapping Debate.
NPs, however, say there is no evidence to support that their diagnostic abilities aren't up to par or they have higher rates of midiagnosis. "If we could not recognize [such cases], you would see a lot more lawsuits against nurse practitioners for not recognizing them, but those lawsuits aren't there," Angela Golden, a clinical nurse practitioner and educator and co-president of the American Association of Nurse Practitioners told Remapping Debate.
But physicians argued that death and malpractice rates aren't proper metrics. Mary Ellen Rimsza, M.D., a practicing pediatrician, professor at the University of Arizona, and chair of the American Academy of Pediatrics' workforce committee, told the publication that it's impossible to assess whether NPs prevent deaths because there are so few nurses practicing independently even in states that allow expanded scope of practice. Most of them work in team-based clinics, she said.
Despite the differences, Remapping Debate said that nearly all doctors and nurses interviewed for their in-depth report agreed that quality of care improved significantly when healthcare professionals work together. However, doctors believe teams need a primary care physician on hand to handle complicated cases.
"Every member of the team is critical," Reid B. Blackwelder, M.D., president of the American Academy of Family Physicians and a practicing family physician in Tennessee, told the publication. "Every member has roles they can play. Some of those roles overlap. But you can't just substitute one member of the team for another.”] For the full article
- And what happens when there isn't any physican to deliver the necessary care (especially in rural areas), however there is a qualified NP?
- This is about positioning, and what side you are on. Pushing the conversation to this level gets away from the real issue….Getting enough qualified practitioners to deliver quality care to those who need it, without putting additional burden on the system or patients themselves.
 The states that have done away with the piece of paper (collaborative agreement, payment to practice without actual information being shared to determine course of individual patient protocol) will continue to grow and create a more effective and efficient system.
The states that have done away with the piece of paper (collaborative agreement, payment to practice without actual information being shared to determine course of individual patient protocol) will continue to grow and create a more effective and efficient system.
It is not ‘IF’, but ‘When’.