Mental Health | The Stages of Grief as a Framework for the Journey
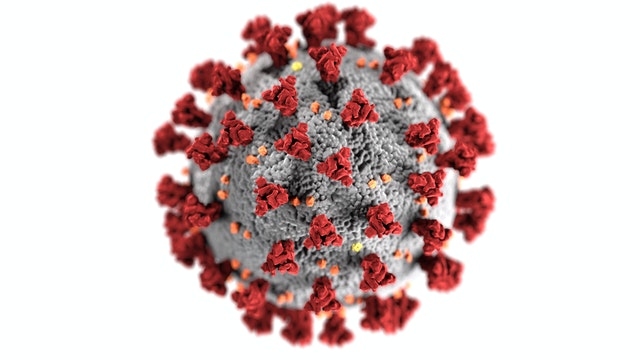
 Mental Health Update | As a health care professional, I have watched the progress of the COVID-19 pandemic with alternating measures of horror, dread, fascination, frustration, and fear.
Mental Health Update | As a health care professional, I have watched the progress of the COVID-19 pandemic with alternating measures of horror, dread, fascination, frustration, and fear.
The nurse in me wants to jump onto the front lines, don scrubs, and volunteer at the nearest emergency room. As I watch the understandable human response to this unprecedented circumstance, I know my skills as a psychiatric clinician will be needed soon enough to help with the emotional impact of this pandemic.
The five stages of grief (denial, anger, bargaining, depression and acceptance), as outlined by psychiatrist Elisabeth Kübler-Ross to describe the emotional journey of preparing for the death of a loved one, plot a useful map as we transit through the uncharted emotional aspects of the COVID-19 pandemic.
For some time, many people—including some in important positions of leadership—appeared to be in denial about the risk of this virus. For many of us, it was an event happening in another part of the world. Concerning, of course, but not immediately impactful. We went about our springtime lives, planning conferences, basketball tournaments, and vacations unaware of what could befall us. Denial always looks foolish in retrospect, but at the time of the threat, as my blogger colleague Dr. Holly Hendin recently noted, denial is adaptive as it permits us to navigate a world of unpredictable threats without becoming paralyzed with fear.
Once denial became untenable (each day I look at the Johns Hopkins dashboard and am astounded at the power of exponential growth curves), our collective anxiety turned to anger and fear of harm and scarcity. The latter led to absurd behaviors—hoarding toilet paper, or worse, hand sanitizer and N95 masks. The latter of these led to genuine, appropriate anger as health care workers were left to improvise personal protective equipment, leading well-intentioned citizens to organize sewing bees to make surgical masks, and we all asked the question “Why didn’t we start preparing sooner?”.
Anger led to bargaining, as we realized the potential harm of this pandemic and the need to enforce social distancing through closure orders of bars and restaurants and, increasingly, shelter-in-place orders that turned some of our largest cities into ghost towns. Stock markets buckled, unemployment claims skyrocketed, and a question began to be asked—can we maintain a healthy economy and still contain COVID-19? How many people would we be willing to allow to perish to continue a robust economy? It’s a perverse version of the runaway trolley problem, except we’re now trying to save the trolley and not the people who lie in its path. All the models of an unmitigated pandemic predict an overwhelmed US medical system, as it was in northern Italy. When that happens, a cruel triage will become essential: who is most deserving of a ventilator or an intensive care unit bed? This is a decision I would not want to faced with, and a moral trauma that I wish to prevent my colleagues from ever having to make. This is why we are staying home and missing out—so that our Emergency Department colleagues don’t have to decide who lives and who dies.
The Road Ahead
So, what lies ahead for us and our patients? It’s not an easy road, and it’s likely to involve a period of depression and post-traumatic reactions before arriving at last to acceptance and growth. But before we get there, we’ll invariably cycle through all the stages of grief again and again, with each new development, with each new loss. While fortunately, I have not yet had to face the grief of losing a loved one to this illness, I and everyone else has lost the normalcy of regular life. I miss seeing my friends, of going out to dinner in a restaurant, to going on a vacation during spring break. Of course, these are minor sacrifices when we are trying to curb a pandemic, and ones that I willingly make, and with each one comes loss. Further still, there is anticipatory anxiety about what losses are coming next. Will our kids finish this school year? Will we lose our jobs? Will family members and friends die? We don’t know. I was talking to a friend this week about her psychotherapy practice during the time of COVID-19. She remarked, “Normally, my patients are working on seeing the irrationality of their fears, but what do you tell someone like that in a time like this?”
I was talking to a friend this week about her psychotherapy practice during the time of COVID-19. She remarked, “Normally, my patients are working on seeing the irrationality of their fears, but what do you tell someone like that in a time like this?”
Indeed, in a time where the pandemic of coronavirus has made shelter-in-place orders essential, everyone and every surface becomes a potential threat. When I walk in my usually bustling San Francisco neighborhood, the streets are eerily quiet, and people cross the street rather than pass on the sidewalk with less than 6 feet separating us. I come home, wash my hands, and hope that somewhere, somehow a virus hasn’t found its way into my respiratory tract.
Addressing Anxiety
What do we tell our patients who are understandably anxious about the pandemic? First of all, tell them their feelings are normal, to be expected. Who wouldn’t feel anxious about a pathogen that can’t be seen, seems to live a long period of time on common surfaces such as doorknobs (this is a really rough time to have obsessive-compulsive disorder), and appears to be infecting the population at a logarithmic rate every 3-6 days? If you’re not anxious, you’re probably not paying attention.
For those who already struggle with anxiety, it may get worse for a while. How could it not?
This excerpt is by Andrew Penn, RN, MS, NP, CNS, APRN-BC


