Attention deficit hyperactivity disorder (ADHD) is one of the most common mental disorders in children and adolescents.
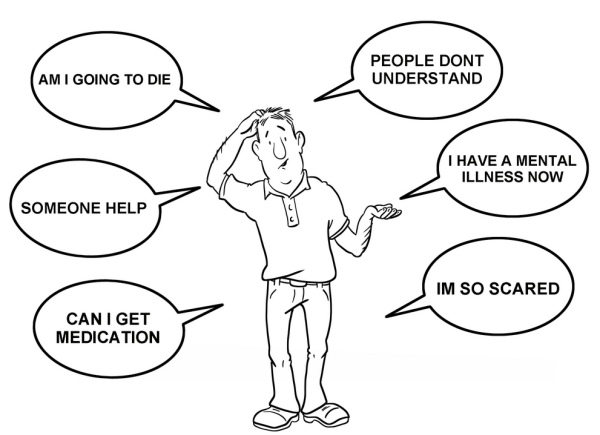
Symptoms include difficulty staying focused and paying attention, difficulty controlling behavior, and very high levels of activity. Studies show that the number of children being diagnosed with ADHD is increasing, but it is unclear why.
Minneapolis Mental Health | Here is how ADHD looked according to the past:
ADHD was seen as a behavioral disturbance caused by environmental factors, such as inconsistent parenting.
Methods to study brain development in people with ADHD were not available.
ADHD was treated with immediate release stimulant medications such as methylphenidate (e.g., Ritalin), which worked well but only lasted for a few hours. Children needed multiple doses during the day, disrupting their school schedules and daily activities.
Here is how ADHD is seen from today’s more developed perspective (and we are not finished finding better and better ways either):
Using brain imaging technology like magnetic resonance imaging (MRI), scientists have observed that in some children, ADHD may be related to how the brain is wired or how it is structured. For other children with ADHD, brain development follows a normal but delayed pattern. In some regions, development is delayed by an average of three years compared to children without the disorder.
The delay appears to be in the frontal cortex, a part of the brain that supports the ability to suppress inappropriate actions and thoughts, focus attention, remember things moment to moment, work for reward, and plan ahead.
In contrast, the motor cortex—the area that controls movement—tends to mature faster than normal in children with ADHD, an exception to the pattern of delay. This mismatch in brain development may account for the restlessness and fidgety symptoms commonly associated with ADHD.
Findings from the Preschoolers with ADHD Treatment Study (PATS) indicate that using a very low dose of methylphenidate (e.g., Ritalin) to treat children 3–5 years old diagnosed with severe ADHD can be effective.
However, for some very young children, early behavioral interventions designed to reduce their ADHD symptoms may be effective alternatives or additions to medication treatment.
Preschoolers with fewer than three coexisting disorders were most likely to respond to methylphenidate treatment, whereas those with three or more coexisting disorders did not respond to the treatment.
Different types of psychotherapy are effective in treating ADHD.
Behavioral therapy helps teach practical skills such as how to organize tasks and manage time to complete homework assignments. It also helps children work through difficult emotions. Therapists also teach children social skills such as how to wait their turn, share toys, ask for help, or respond to teasing.
Studies show that interventions that include intensive parent education programs can help decrease ADHD problem behavior because parents are better educated about the disorder and better prepared to manage their child’s symptoms. They are taught organizational skills and how to develop and keep a schedule for their child. They are also taught how to give immediate and positive feedback for behaviors they want to encourage, and how to ignore or immediately redirect behaviors they want to discourage.
The Multimodal Treatment Study of Children with ADHD (MTA study) is helping to inform long-term treatment decisions. For example, MTA researchers found that medication works best when treatment is regularly monitored by the prescribing doctor and the dose is adjusted based on the child’s needs. As children with ADHD mature, treatment decisions should adapt to the demands of adolescence and take into account long-term academic and behavioral problems commonly associated with ADHD.
ADHD likely stems from interactions between genes and environmental or non-genetic factors. Several genes have been implicated in the risk for developing ADHD. One study showed that brain areas controlling attention were thinnest in children with ADHD who carried a particular version of a gene associated with brain development. However, these brain areas normalized in thickness during the teen years, coinciding with clinical improvement. Although this particular gene version increased risk for ADHD, it also predicted better clinical outcomes and higher IQ than two other versions of the same gene in youth with ADHD.
Today and into the future for ADHD therapies: